Angioplasty is an interventional procedure used to open narrow or blocked coronary arteries so blood flow can be restored to the heart muscle without open-heart surgery. This method is also called percutaneous coronary intervention (PCI).
This procedure may be performed during a diagnostic cardiac catheterization when a blockage is detected, or it may be scheduled as a staged procedure after the diagnostic catheterization is performed either during the same hospital stay or at a later date.
Angioplasty begins the same way as a cardiac catheterization. This procedure is sometimes called “balloon angioplasty”, which is usually done in combination with stenting.
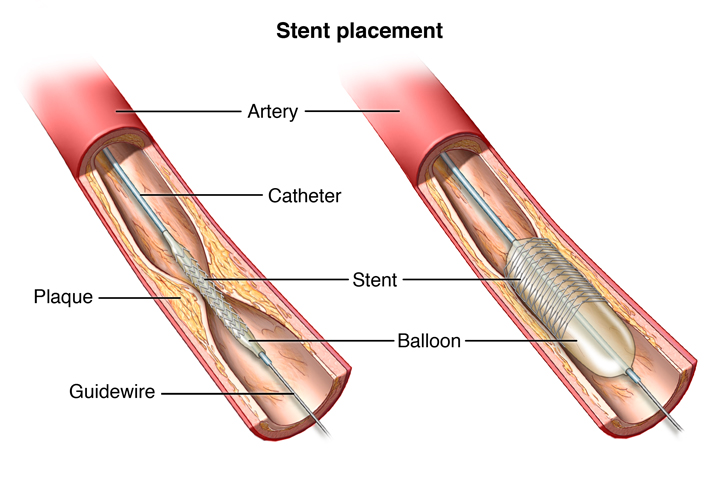
Just like cardiac catheterization, a catheter is placed through the femoral artery into the heart. If it is determined that significant heart disease is present, the physician determines the need for balloon angioplasty and stent placement.
With balloon angioplasty, a small balloon at the tip of the catheter is inserted near the blocked or narrowed area of the coronary artery. When the balloon is inflated, the plaque or blockage is compressed against the artery walls and the diameter of the blood vessel is enlarged to increase blood flow to the heart. In most cases, a stent is used for a more permanent solution. A stent is a small, metal mesh tube that provides a framework of support inside the coronary artery. A balloon catheter is then used to insert the stent into the narrowed artery. Once in place, the balloon is inflated, the stent expands and holds the artery open. The balloon is then deflated and removed, while the stent stays in place permanently. Over a period of several weeks, the artery heals around the stent. With this technique, re-occurrence of narrowing of the arteries (restenosis) is somewhat diminished.
Once the stent has been placed, tissue will begin to form over it within a few days or weeks after the procedure. The stent will be completely covered by scar tissue within months, depending upon the type of stent placed. As needed, Dr. Fenster will prescribe a blood-thinning medication to keep blood clots from forming inside the stent. You will be taking this for several months to years after your procedure to prevent the risk of clotting in the stent. It is extremely important to keep taking the medications as prescribed until Dr. Fenster tells you otherwise.
What happens if…?
If you experience any chest pain or unexpected discomfort after you leave the hospital, immediately call 911 and go to the nearest hospital for evaluation.
It is possible for scar tissue to form inside the stent. If this happens, a repeat procedure may be needed, either with balloon angioplasty or with a second stent.
Angioplasty with stenting is most commonly recommended for patients who have a blockage in one or two coronary arteries. If there are blockages in more than two coronary arteries, coronary artery bypass surgery may be recommended.
What are the risks?
Coronary angiography is a common medical procedure. The risk of complications is higher in people who are older and in those who have certain diseases or conditions (such as chronic kidney disease and diabetes).
Possible complications may include but are not limited to:
-Chest pain/angina, bleeding, or infection
-Blood vessel damage (at times requiring immediate surgery)
-Reaction to the dye if allergic or have kidney disease
-Heart attack
-Stroke
-Death
How do I prepare for angioplasty?
Please discuss these following recommendations with Dr. Fenster prior to your procedure. Please arrive at the hospital’s outpatient entrance to register at the time requested, making sure you bring your insurance cards and picture identification with you.
- DO NOT eat or drink anything after midnight the night before your procedure.
- Take the following medications the morning of your procedure with a sip of water (unless your doctor has told you otherwise):
*Heart and blood pressure medications
*Plavix and aspirin if they have been prescribed to you
DO NOT take the following medications:
*Diabetic medications, including Glucophage. Stop taking the night before the procedure.
*Coumadin (unless your doctor instructed you to take it) – stop three days prior to procedure
*Xarelto – stop 1 day prior to procedure
*Pradaxa – stop two days prior to procedure
*Diuretic medications/“Water pill” such as Lasix or Hydrochorothiazide. Do not take the morning of procedure; you may resume the evening after your procedure.
Bring a list of ALL medications, including over the counter medications. Include dosage and times you take them.
- Take a shower the night before or the morning of your procedure.
- Please leave ALL valuables at home.
- If you become sick with any virus, sore throat, temperature/fever, or cough, notify your cardiologist prior to coming to the hospital.
- Make sure your have an emergency contact with their phone number.
- You will NOT be able to drive yourself home, so make sure you have a responsible person to drive you home.
- Make sure to have your lab work drawn 2-3 days prior to the cardiac catheterization. These can be drawn at the lab or hospital of your choice. A prescription for the lab will be provided to you.
Questions?
If you have any questions concerning your procedure, please contact the Cardiac Institute of the Palm Beaches at (561) 296-5225.
American Heart Association: What is Coronary Angioplasty?
Recovering from angioplasty: Things you should know after your stent placement.
NIH: What to expect after angioplasty.